Professor Ben Bridgewater: Determining my cancer risk

In his fifth blog of his personal health challenge series, our Chief Executive Professor Ben Bridgewater reflects on his health journey so far and looks to determine his cancer risk.
Over the last few weeks in this series of blogs, I have assessed my health and wellness online, reassured myself that I am not in bad shape and put some things in place to decrease my risk of diabetes – which will also benefit my health in other ways. I have also only shelled out £14.99, for a blood glucose monitor. I have assessed of my overall wellness using online tools and, as a result, targeted some changes in other aspect of my life.
So far, I am finding it all beneficial – specifically I have lost 12 lbs over three weeks, just by monitoring and restricting my calorie intake and hitting a step target of at least 10,000 steps a day. I have not found the steps too much of a challenge as I have simply been walking while I have conference calls at work wherever possible and walking to do whatever chores I have to do at weekends. I have incorporated mindfulness into my walking rituals and do strengthening exercises a few times a week. I feel leaner physically and more effective mentally as a consequence. My wife and kids are all happy with the changes in place – my wife because I am not so fat, and my kids because we are spending more time together walking to pub and chatting.
I think I have taken things as far as I can responsibly go without seeking medical help, and while I am pretty comfortable now about my cardiovascular health and risk factors, the other major killers for men in the their 50s include respiratory disease, lung cancer, colorectal cancer and liver disease. For men in their 60s prostate cancer is added to the mix.
I now plan to go to see my GP and will book an appointment, and there are really two things I want to talk to them about:
- Does it make sense for me to have any screening for the common cancers?
- I have spent a bit too much time in the sun in my life and have a couple of skin things on my scalp, which I have had for many years, for which I need professional advice. The second of these is straightforward I think. I have thought about taking some pictures and using an online telemedicine service, but I think this is taking technology and individual empowerment too far for me at the moment.
So what about cancer?
Lung cancer is common, with the major risk factor being smoking. I have never smoked and so my risk for this is low. Bowel cancer is the third most common cancer in men, after lung and prostate, with these three cancers contributing to just under half of all cancers worldwide. When diagnosed at its earliest stage, more than nine in 10 people with bowel cancer will survive their disease for five years or more, compared with one in 10 when the disease is diagnosed at the later stages. Five-year survival for colon cancer in men is below the European average in England, presumably because it is diagnosed late.
The causes of bowel cancer are not completely understood but the risk factors include your age, family history of bowel cancer in a first degree relative (I do not have this), your diet (high in red and processed meat and low in fibre), excess alcohol (I don’t drink often), obesity (I have already taken action on this), inactivity (again, I have been increasing my activity levels), digestive disorders (I do not have any), and various rare genetic conditions (no).

I struggled a little to find a useful online calculator to assess my personal risk, and the best I could come up with was from Ontario in Canada and the results indicate my personal status is average, with a lifetime risk of one in 14 – this seems high. The recommendations include eating less red or processed meat, eating/drinking more dairy products and increasing the amount of food and vegetables in my die. By messing around with the calculator online I understand that I can decrease my risk, but cannot get a quantified assessment of how much my risk would decrease, which is a shame as I found the actual numbers in my diabetes assessment to be useful as an incentive to lose weight.
Colorectal cancer is one of the cancers (like breast cancer) which has a national screening programme in place. The NHS offers bowel cancer screening using a home testing kit to everyone in England from the age of 60 and it examines evidence of cancer in the faeces. Screening is offered every two years between the ages of 60 and 74, so I am not old enough yet to be offered this service, and given my risk is not elevated and I am not unduly anxious about this so there seems to be no need to push this further. Bowel scope screening is also being rolled out using a telescope for people over 55, but this is not yet offered in the area where I live, so there is a postcode lottery here.
Prostate cancer is the other significant risk. It is the most common cancer in men in the UK, with 130 new cases being diagnosed every day. It usually develops slowly, so there may be no signs of the disease for many years. Prostate cancer accounts for 26% of all new cancer cases in men and the incidence goes up with increasing age. The incidence is also increasing over time and about 40% of prostate cancers are diagnosed late in the disease when treatments are less effective. Overall 84% of men with prostate cancer survive for 10 years or more, but survival rates for people diagnosed in their 50s and 60s are better than in older people. As with most cancers, diagnosis of early stage disease is associated with better outcomes.
Family history is important in determining your risk of prostate cancer. If someone has one direct relative with prostate cancer he is twice as likely to get the disease as someone with no such history; if he has two close male relatives the risk goes up to five times higher. I have no family history of prostate cancer, but my wife does and, as a consequence, she is repeatedly suggesting I get a test done.
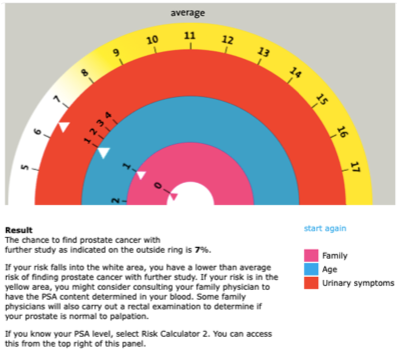
To get a quantifiable assessment of my risk on this I have used a prostate cancer risk calculator, which asks about you age, your family history and your urinary symptoms. My risk on this is low (and as low as it can be for a man of my age). But according to the calculator there is a one in 14 chance of finding prostate cancer on further investigations.
As it stands there seems to be no evidence that the benefit of prostate cancer screening outweigh the risks, and so there is not national programme in place for this. It is possible to measure a substance in the blood – the prostate specific antigen PSA – which is associated with prostate cancer, but the test is unreliable and can suggest cancer when none exists (a false positive test) or incorrectly suggest no cancer in about 15% of men (false negative test).
Having a PSA test can lead to unpleasant further tests, and very difficult decisions about treatment options. The current NHS policy on PSA testing for otherwise healthy men over 50 is a so called “informed choice programme” which requires a sensible chat between the patient and the doctor about the pros and cons. If my risk was elevated I am sure I would have the test – given it is not I will chat about this to my GP and factor in my wife’s perspective to the conversation.
So my next stage is to book a GP appointment to discuss my health. I will report back on this in my next blog and I will summarise what I have learned during this attempt to empower my health and wellbeing with technology.


