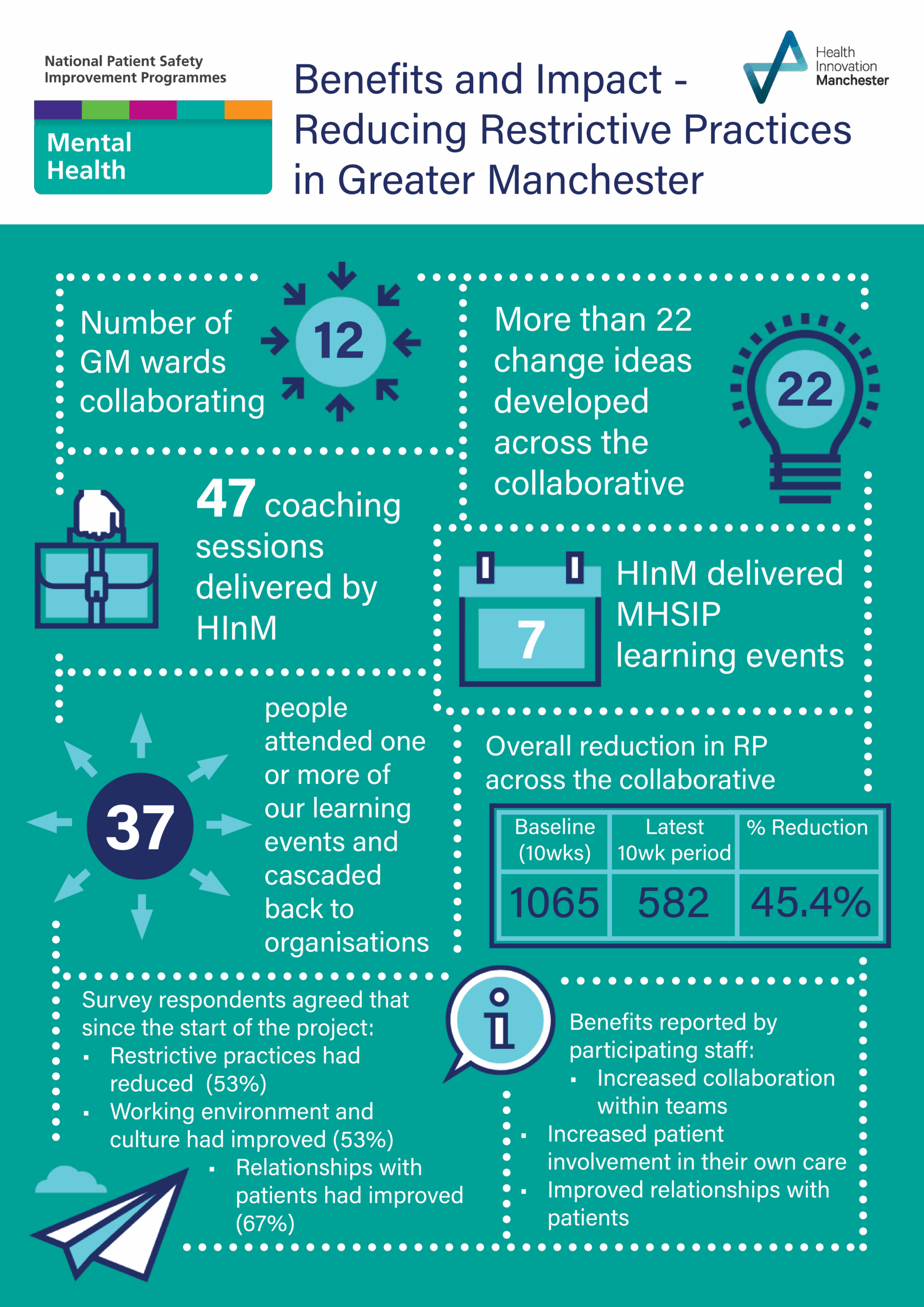
Patient Safety Collaborative (GMECPSC) – Mental Health
PSCs bring together people and organisations to transform the health and wellbeing of the population. The PSCs are part of the 15 Academic Health Science Networks (AHSNs) across England running this programme for their region.
With partners from the NHS, social care, and academia, we support improvements in discovery science, innovation into practice, patient safety and population health and focus where the need and benefit are greatest. Using systematic quality improvement methodology to deliver innovation and improvement at scale and pace.
Beyond serving the local population, healthcare solutions developed by members are also applied across the UK and globally.
Background
The Mental Health Safety Improvement Programme (MHSIP) aims to improve safety by reducing harm caused to people using mental health, learning disabilities and autism inpatient services by 2024.
Restrictive practice refers to any act which involves restricting a person such as physical restraint, the use of rapid tranquillisation, or the use of a seclusion room.
The Mental Health Safety Improvement programme involves rolling out a tried and tested change package for reducing restrictive practice. The change package is based on a pilot undertaken by the National Collaborating Centre for Mental Health.
This project was part of the national mandated patient safety commission from NHS England. The Greater Manchester and Eastern Cheshire Patient Safety Collaborative (PSC) has supported the Greater Manchester (GM) health and care system to bring about systematic and sustainable improvement in patient safety by utilising quality improvement approaches and methodology.
This programme brought together teams from different Mental Health Trusts, other providers and partners, across a range of specialities and roles who all had in common enthusiasm, motivation, and capability to drive patient safety improvements in their organisation for the benefit of their patients and staff.
Why restrictive practice?
Restrictive practices cause both physical and psychological harm to patients and are often retraumatising to an already vulnerable patient group. The use of restrictive practice can impact negatively on staff who either use restrictive interventions on patients themselves or who witness them. Wards with high levels of restrictive practices often have unstable staff groups, heavily supported by agency staff, and can often have difficulties recruiting and retaining staff. They can be difficult places for patients and staff to stay or work on, which is counterproductive to building the trusting relationships between staff and patients that are fundamental to safe high-quality mental health care.
There is large variation between like services in rates of restrictive practice, and marked inequality in race, diagnosis, age and sex. The CQC’s 2017 State of Care review of mental health and learning disability services observe and report this large variation in practice, and the recently published Department of Health and Social Care’s Mental Health Units (Use of Force) Act 2018 statutory guidance reports that there is still work to do.
The Mental Health Units (Use of Force) Act 2018 , came into being after Olaseni Lewis, a young black man, died as a result of restraint whilst using mental health services. This programme delivers the cores changes described within this act; ‘changes to promote positive ward cultures which support recovery, engenders trust between patients and staff, and protects the safety and wellbeing of all our patients and people using our mental health services.’ (Department of Health and Social Care, 2021) .
Methodology
Teams were coached in quality improvement methodology based on the Model for Improvement, developed by the Associates in Process Improvement. Source: Langley GL, Moen R, Nolan KM, Nolan TW, Norman CL, Provost LP. The Improvement Guide: A Practical Approach to Enhancing Organizational Performance (2nd edition). San Francisco: Jossey-Bass Publishers; 2009.
This is an extremely simple and user-friendly model that ensures 3 basic building blocks are in place:
- Project aim (What are we trying to accomplish?)
- A measurement system (How will we know that change is an improvement?)
- Change ideas and a theory for change (What change can we make that will result in improvement?)
‘Plan, do, study, act’ (PDSA) cycles are then used to test change ideas and evaluate results as teams progress.

Programme Aim and Theory for Change
The aims of our programme in Greater Manchester were:
- National target of 25% reduction in incidence of restrictive practice in all inpatient mental health, learning disabilities and autism wards engaged in the programme, including the networks, by April 2023.
- To support at least 10% of eligible inpatient mental health, learning disabilities and autism wards in Greater Manchester.
In 2018, a pilot, run by the National Collaborating Centre for Mental Health (NCCMH), supported 38 inpatient mental health wards across England to reduce their use of restrictive practice using a quality improvement approach. The output of this work provided a tried and tested change package to be rolled out across England as part of the MHSIP.
Find out more about the NCCMH pilot here.
National resources to support the MHSIP can be found here. These include a driver diagram, measurement plan, details of tried and tested change ideas and shared templates and resources.
A workspace was also set up on FutureNHS to support teams nationally. View the workspace here.
All PSCs across England worked to the same theory for change within the MHSIP, based on the work of the NCCMH pilot. This theory for change is explained by the driver diagram below.

Measurement Strategy

We adopted the measurement strategy suggested by the national MHSIP (see left and here).
Each participating ward was required to capture data to measure 3 main outcomes:
- The number of episodes of physical restraint
- The number of episodes of seclusion
- The number of times that rapid tranquillisation is administered
Operational definitions were provided by the national MHSIP (see right and here). Some participating wards already routinely collected these measures via there existing electronic recording systems and were therefore able to run regular reports for the benefit of the improvement teams. Where these data were not already routinely collected, we encouraged participating wards to use safety crosses to capture raw data which was then fed into a spreadsheet.
The 3 measures above could be aggregated into a single combined, headline measure: The number of all restrictive practices per month.
In addition to the stipulated measures above, one ward initiated two additional measures to gain a deeper insight into the impact of changes made on the ward:
- In addition to the number of incidents of seclusion, measuring the daily or weekly amount of time spent by patients in seclusion
- Measuring the daily or weekly number of verbal ‘de-escalations’ as a leading measure of activity to avoid restrictive practices
Where, possible we tried to collect the following data items in order to monitor the effect of staffing on use of RPs:
- Number of permanent employees who have left the organisation in the reporting month
- Number of agency staff employed on the ward in the reporting month
- Number of bank staff employed on the ward in the reporting month
- Percentage of staff sickness in the reporting month
Data Analysis
In this video clip, Andy Holden, Business Analyst at Health Innovation Manchester talks about some of the tools and techniques that were employed in the MHSIP to capture and make best use of data.
Change Ideas
Teams participating in this collaborative were able to benefit from the change ideas published from the 2018 pilot, referred to earlier, as a starting point.
A great number of change ideas were explored as part of this pilot and teams used PDSA cycles to learn about how best to tailor changes to the needs of their own wards.
- DASA tool
- Staff wellbeing pack
- One page patient profiles
- Sensory room
- Ward redesign (bed drop) to accommodate sensory room and activity space
- Use of physical space to transform therapeutic environment
- Refurbishment of seclusion room
- Sensory box
- Purchase kitchen equipment and work with OTs to run baking and healthy eating sessions
- Daily/weekly activity timetable
- Morning meeting with patients to co-develop activity plan
- Challenging unwritten rules e.g.
- Access to garden
- Opening hours of lounge
- Smoking breaks
- Data visualisation
- Safety huddles, with focus on data for improvement
- 1:1 anger management work
- Debriefs following RP incidents
- More open communication with patients to make RP the last resort
- Updating patient information to set realistic expectations about time on the ward
- Heat maps
- Focus on trauma-informed care
- Staff debriefs
- Staff wellbeing focus
Results
Overall we have seen a reduction in all types of restrictive practices across the wards (See table)
In addition to the reduction seen in restrictive practices, there have been a range of additional positive outcomes:
- Improved ward atmosphere has been noticed (anecdotal)
- Programme participation has contributed to staff wellbeing, e.g.
- Time out or ‘headspace’ from clinical practice to reflect on situations
- Investment in development of knowledge and skills
- Empowerment to make better decisions
- The profile and importance of reducing restrictive practice work has increased
- Data quality issues are being addressed within organisations
- Wards are receiving investment in improved facilities
As part of our programme evaluation, we surveyed staff who participated in the programme. The evaluation report can be viewed here. Headline findings are:
- Overall staff felt supported during the programme
- Overall, staff perceived a positive impact on:
- Reducing incidents of restrictive practices
- Improving the working environment and culture
- Improving staff relationships with patients
- Other benefits have included:
- Increased collaboration as a team
- Increased patient involvement in their own care
- Improved knowledge of restrictive practice
| Restrictive Practice Type | Baseline (10wks) | Latest 10wk period | % reduction |
|---|---|---|---|
| Physical Restraint | 764 |
465 |
39.1% |
| Seclusion | 74 |
25 |
66.2% |
| Rapid Tranquilisation | 227 |
92 |
59.5% |
| All types of restrictive practice | 1065 | 582 | 45.4% |
Case Studies and testimonials
We have developed a range of change stories which can be viewed below
What staff have told us about the programme:
Appendices and resources
REsTRAIN Yourself Toolkit (Courtesy of REsTRAIN Yourself programme)
Team Wellbeing Huddle Guide (Courtesy of Aqua)
Practical Post Incident Support (Source: Restraint Reduction Network)
My Support Plan (Source: Restraint Reduction Network)
Post Incident Debriefing Guidance (Source: Restraint Reduction Network)
Example Patient Profile Template
Example Patient Information Sheet
Blanket and Unwritten Rules Presentation (courtesy of Aqua)
Blogs
Reflections on the Mental Health Service Improvement Programme – Stuart Kaill, Programme Development Lead, Health Innovation Manchester
Reflections of an improvement coach in reducing restrictive practice in mental health in-patient settings across the North West of England – Paul Greenwood, Programme Manager, Aqua



















