Chantal Knight: PReCePT and sustainability of innovation in healthcare services

As part of Patient Safety Awareness Week, Chantal Knight, Maternity Safety Lead for Greater Manchester and Eastern Cheshire Strategic Clinical Networks and Health Innovation Manchester, explains how implementing sustainable innovation and change within services must be focussed on embedding it within the organisation and staff.

As an experienced Community Midwife working in rural Cumbria for many years, change management and sustainability of a project were never concepts I was familiar with.
With the nearest Consultant-led maternity unit 35 miles away and a high level of home births in remote locations, I became extremely self-sufficient and creative in my working day.
Friendly farmers also came in very useful for directions and even tow ropes to pull you out of the snow if required!
Changes in management and related practices filtered down slowly and only in a diluted and fragmented way. It was rarely explained as to the WHY and reasoning behind any change, which created a culture at times of resistance and poor take-up of new ways of working. Having this experience has enhanced my understanding of getting staff ‘on side’ when introducing new projects and the importance of planning any innovation.
In my current role as Maternity Safety lead across the Greater Manchester and Eastern Cheshire Strategic Clinical Networks and the Greater Manchester and Eastern Cheshire Patient Safety Collaborative, part of Health Innovation Manchester, I was asked to explore and compare the sustainability of projects in maternity healthcare to see what we could learn for future innovations.
Any change to practice requires careful planning and a clear implementation plan so ownership and commitment are key drivers to ensure success both from the leadership implementing the change to the workers completing the task.
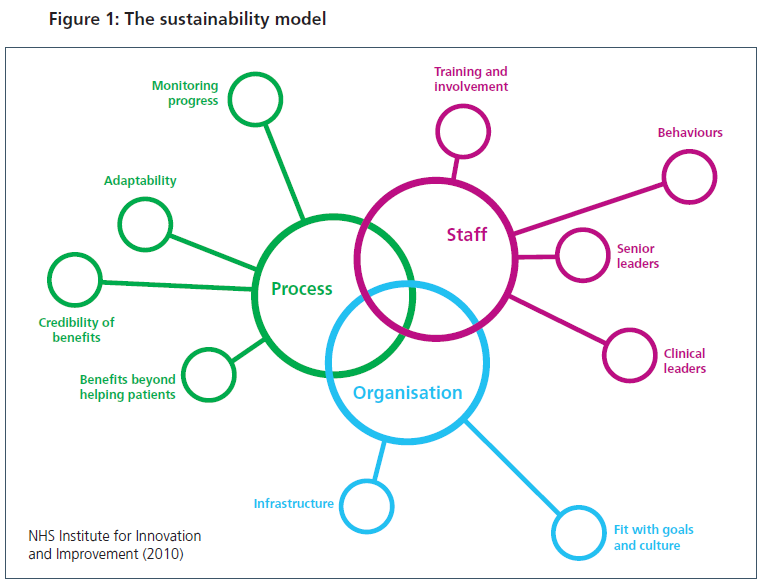
I examined the implementation of the PReCePT programme and used the NHS Improvement Sustainability Model Tool to benchmark the innovation assessing 3 key elements – Process, Staff and Organisation.
Each element drills down to important components which require involvement to assure success and sustainability giving them a score which when collated showed the PReCePT programme with a superior score.

The PReCePT programme aims to ensure at least 85% of all eligible mothers in preterm labour are receiving magnesium sulphate across all maternity units in England by 2020.
Magnesium sulphate protects the baby’s brain and can reduce the risk of cerebral palsy by 30%, with each individual dose costing £1. Successful scaling up of PReCePT, an evidence-based, cost-effective project, is likely to prevent several hundred cases of cerebral palsy per year, based on highest grade evidence.
Health Innovation Manchester, as an Academic Health Science Network, has been working with maternity units in Greater Manchester and East Cheshire to implement PReCePT as part of a national innovation programme with the AHSN Network. PReCePT has benefitted from this national steer and with a very well-resourced programme produced to assist a successful implementation of the initiative.
There is much to learn from the implementation of the PReCePT programme, especially with the decision initially to launch as a small-scale project, which allowed significant learning when the roll out was presented nationally. Every area of the three elements were incorporated and addressed as activities in the programme with a positive sustained outcome.
Approximately 18 cases of cerebral palsy have been prevented in babies who were eligible across Greater Manchester and East Cheshire from 2015 to 2019 with seven of these cases in 2019. This has improved outcomes for babies and their families, and supported savings of £90 million in ongoing health costs (estimated cost of care of each case of cerebral palsy at £5 million.)
During my role with SCN and Health Innovation Manchester, I’ve realised that innovation in healthcare needs to incorporate staff, organisations and processes to ensure it is sustainable in the long-term. Staff need to clearly understand the reasoning behind change and innovations need to be fully evidenced and resources to support implementation.
It is also not just large scale innovations where these ideas can be seen in practice. I look back to my days working clinically and reflect on many projects I have been involved with and I can now see that much of my work incorporated many aspects of the NHSI assessment tool.
My role as a supervisor of midwives incorporated assisting women to achieve the birth experience of their choice, even if they were deemed high risk or ‘alternative’ in nature. I can now assess these as actual projects and they incorporated many of the features required to be successful in the NHSI assessment tool especially adaptability, training and senior leadership involvement. Plans would be made, however as we know in maternity care these can change sometimes quite dramatically, but communication was key to ensure the safety of mother and baby with buy in of all key staff. The positive long term physical and mental health outcomes for mum and baby could not be overestimated if the delivery was a success in the mother’s eyes and I am proud to say I have witnessed many.


