CVD Prevention
Resources for Health and Care
The following resources are for health and care professionals, and are being shared as part of the Greater Manchester Integrated Care Systems CVD Prevention initiative. For information or support, please contact [email protected].
CVD Prevention Toolkits for Health and Care professionals in Greater Manchester
A range of CVD Prevention Toolkits for Health and Care professionals in Greater Manchester have been created in collaboration with NHS GM Integrated Care, Health Innovation Manchester, the Greater Manchester and Eastern Cheshire Strategic Clinical Networks, the Greater Manchester Neurorehabilitation and Integrated Stroke Delivery Network, and the North West Kidney Network. Bookmark resources.gmcvd.com to easily access the latest CVD Prevention Resources.
Click on each image below to access each toolkit.
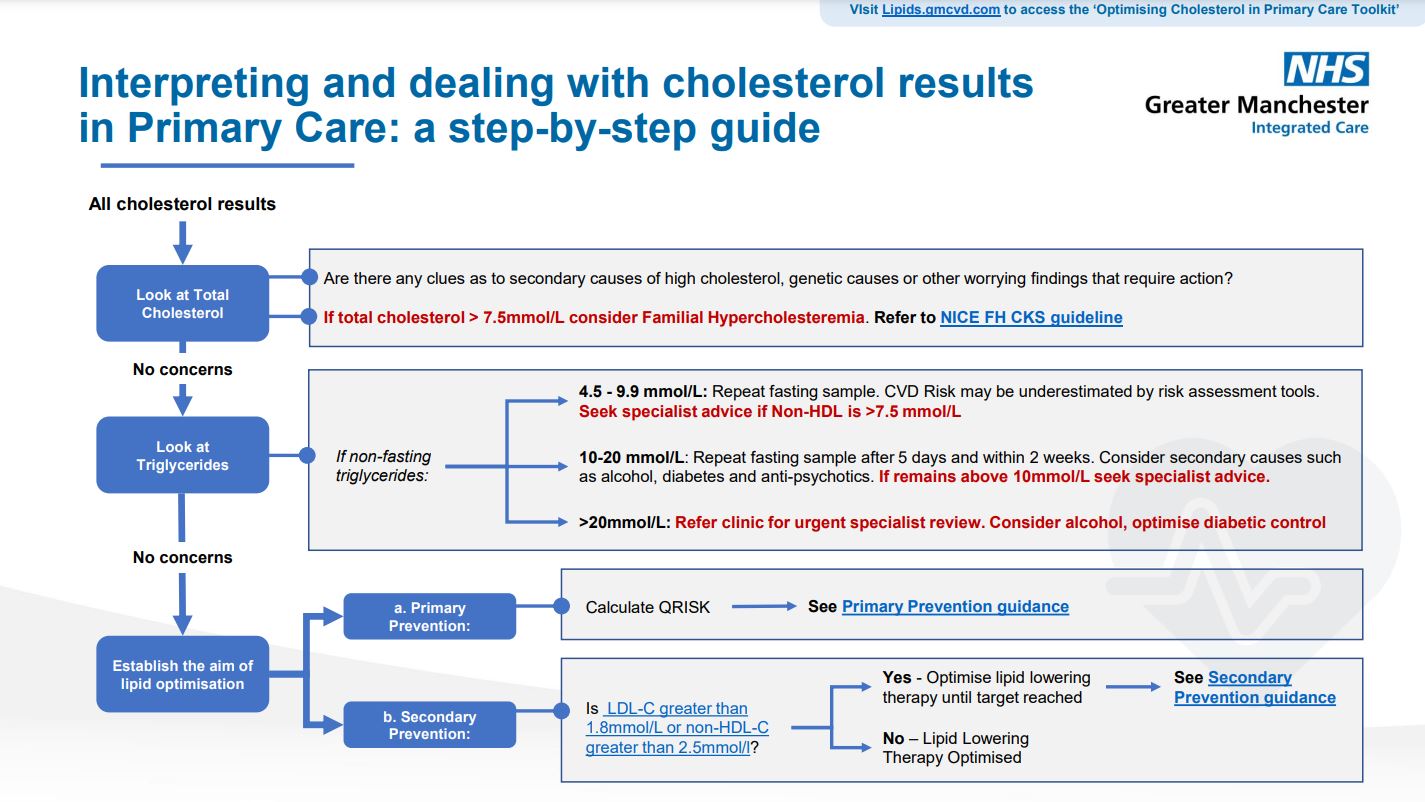
Lipid Management Pathway for the Secondary Prevention of CVD
Lipid Management Pathway Education Webinars
Lipid Management Webinar
Click here to access the pdf of the Lipid Management Webinar.
Chapter Shortcuts
Chapter 1: Importance of Lowering Cholesterol
Chapter 2: What’s in the Lipid Profile?
Chapter 3: Lipid Management Pathways
Chapter 4: Statins and Statin Intolerance
Chapter 5: Lipid Lowering Therapies
Chapter 6: Optimising Lipid Treatment in CVD
Chapter 7: Familial Hypocholesterolaemia
Chapter 8: Hypertriglyceridemia
Chapter 9: Case Finding
Case Finding and Searches
Searches for the identification of high-risk people requiring lipid optimisation for secondary prevention of CVD have been developed.
The searches risk-stratify patients into five cohort groups depending on intervention required and includes eligibility for injectable therapies.
Disclaimer:
‘Greater Manchester CVD Prevention- Lipids Searches’ have been created by Greater Manchester Integrated Care Partnership and are proprietary to Greater Manchester Integrated Care Partnership. By downloading and running the ‘Greater Manchester CVD Prevention- Lipids Searches’, users confirm:
- That the search tools must be used in accordance with any instructions supplied by Greater Manchester Integrated Care Partnership.
- You understand the criteria on which they are based.
- You understand the search tools can only identify those patients who have been correctly coded into the Electronic Health Record. Greater Manchester Integrated Care Partnership is not responsible for primary care health record coding.
- You will acknowledge Greater Manchester Integrated Care Partnership in any communications with third parties and the public about this work.
- Except to the extent our liability cannot be excluded by law, assume full responsibility for all decision and consequences of implementing the search and stratification tools along with the wider framework.
- That you will not use or exploit these tools for research or commercial gain.
Adaptation of the search tools by primary care teams (e.g. PCN/ GP Practice/ ICS):
The ‘Greater Manchester CVD Prevention- Lipids Searches’ have been created specifically for Greater Manchester Integrated Care Partnership. Therefore, additional validations will be required by PCN/ GP practice/ ICS when adapting the search.
Primary Care/ PCN users are able to amend the search and stratification tools to reflect local preferences. In such instances, Greater Manchester Integrated Care Partnership is not responsible for any outputs. In this case users must state that they have adapted the ‘Greater Manchester CVD Prevention- Lipids Searches’. Suggested wording: “Adapted from Greater Manchester CVD Prevention- Lipids Searches.”
Adaptation of the search tools by suppliers:
Adaptation by distributors (e.g. organisations that share templates to other organisations) must replicate the ‘Greater Manchester CVD Prevention- Lipids Searches’ in entirety without adaptation. Where they wish to adapt the frameworks, they must contact Greater Manchester Integrated Care Partnership for permission.
Guidance documents for searches are available for download on the links below.
Case Finding and Searches Using TPP/SystmOne
Case Finding and Searches Using EMIS
Case Finding and Searches Using InPS Vision
Lab coding issues
This suite of searches (below) includes total cholesterol values where there may be local lab coding issues for LDL / Non-HDL results. Please only use this set of searches if there are coding issues
Inclisiran Prescribing, Ordering and Cost Information
Please find further information on https://www.england.nhs.uk/publication/cvd-prevention-lipid-management-inclisiran/
Further Resources
Heart UK have a variety of resources available for health professionals working with lipid conditions:
- Resources for healthcare professionals: access here.
- Tackling Cholesterol Together: HEART UK has partnered with the NHS Accelerated Access Collaborative (AAC) and the Health Innovation Network to provide a comprehensive and varied education programme for healthcare professionals. Access resources here.
- Resources for patients: access information for patients on cholesterol here
Podcast: Cholesterol Management in General Practice
The ‘Primary Care Knowledge Boost’ podcast aims to improve the confidence and knowledge of local primary care clinicians through interviews with specialists from around Greater Manchester.
Dr Aseem Mishra is an Academic GP trainee who has been involved in helping produce the Guidelines for the Greater Manchester Lipid Pathway. Dr Mishra talks through guidelines for how to treat hyperlipidaemia, recent changes to these guidelines, and injectable treatments for secondary prevention. Follow the link to listen and access further resources.