Patient Safety Collaborative (GMPSC) – Maternity and Neonatal

As a key component of the NHS Patient Safety Strategy, the National Patient Safety Improvement Programmes address the most important safety issues and embed improvement methods and measurement into systems
The 15 national Patient Safety Collaboratives (PSCs) will support Integrated Care Systems (ICS’s) to deliver the national programmes
In Greater Manchester (GM) the Maternity and Neonatal Safety Improvement Programme (MatNeoSIP) is delivered by Health Innovation Manchester (HInM) under the leadership of Stuart Kaill (Senior Programme Development Lead), Caroline Finch (Programme Development Lead) and Rebecca Williams (Project Manager)
MatNeoSIP Mission
The mission of MatNeoSIP is to create and embed the conditions for all staff to improve safety and outcomes of maternal and neonatal care by reducing unwarranted variation and providing a high-quality healthcare experience for all women, babies and families across England.
MatNeoSIP Key ambitions:
- to improve the optimisation and stabilisation of the preterm infant
- strengthen the prevention, identification, escalation, and response (PIER) to maternal and neonatal deterioration
- use safety culture insights for improved quality of care and inform local improvement plans
- avoiding brain injury in childbirth (ABC)
All eight of GM Local Maternity and Neonatal System (LMNS) providers will be supported by HInM to deliver on the NHSE (NHS England) commissioned safety improvement work. Supporting the teams and working with key system stakeholders who are focussed on the safe, personal, and effective care of our birthing people and their families. The GM PSC (Patient Safety Collaborative) approach to the delivery of the MatNeoSIP is as follows
Areas of Improvement
All nine of GM Local Maternity and Neonatal System (LMNS) providers will be supported by HInM to deliver on the NHSE (NHS England) commissioned safety improvement work. Supporting the teams and working with key system stakeholders who are focussed on the safe, personal, and effective care of our birthing people and their families. The GM PSC (Patient Safety Collaborative) approach to the delivery of the MatNeoSIP is as follows
We are collaborating with the Quality Improvement Lead Nurse for the Northwest Neonatal Operational Delivery Network (NWNODN).
We will continue to work directly with optimisation teams to deliver and embed the nine key evidenced based preterm perinatal optimisation interventions that are proven to improve outcomes.
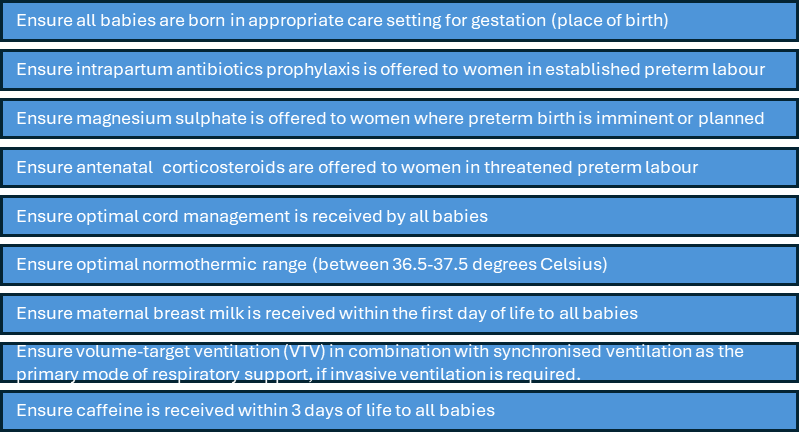
There is compelling evidence that babies who receive all the appropriate aspects of the interventions have improved outcomes. The British Association of Perinatal Medicine (BAPM) have released a perinatal quality improvement (QI) package to support maternity and neonatal providers to implement. Further information can be found here.
Further information can be found on our FutureNHS page
For our up to date leaflet ‘Improving the outcome for preterm babies: information for parents’ click here.
Maternity Early Warning Score (MEWS)
NHS England has commissioned the national roll out of standardised, evidence-based Maternity Early Warning Score (MEWS) tool, designed around the psychological changes of pregnancy and informed by robust UK population data. Implementation will ensure that all staff and those cared for by maternity services benefit from a clear evidence-based system – and a common language to help escalate concerns.
The national patient safety team have launched three MEWS podcasts which describe how the tool has been developed, discuss the benefits of a standardised approach to reduce variation and discusses feedback from pilot of the tool.
Podcast One: Maternity Early Warning Score – Podcast 1 by NHS England
Podcast Two: Maternity Early Warning Score – Podcast 2 by NHS England
Podcast Three: National Maternity Early Warning Score : Podcast 3 by NHS England
Newborn Early Warning Score Trigger and Track (NEWTT2)
This involves ensuring the NEWTT2 is embedded within an effective PIER pathway for managing deterioration with the aim of improved recognition of deterioration that can leads to interventions and admission the neonatal unit. Early implementation was aimed at providers who do not have a digital system for recording neonatal observations
Further information on NEWTT2 can be found here
Currently we have NEWTT2 implemented in
- East Cheshire NHS Trust
- Tameside and Glossop Integrated Care NHS Foundation Trust
- Wrightington, Wigan and Leigh Teaching Hospitals NHS Foundation Trust
Additional resources can be found with our FutureNHS workspace.
The Perinatal Culture and Leadership Programme (PCLP) aims to improve the quality of care by enabling leaders to drive change with a better understanding of the relationship between leadership, safety improvement and safety culture. The programme supports perinatal leadership teams to create and craft the conditions for a positive culture of safety and continuous improvement, enabling a more psychologically safe, collaborative, and supportive workplace.
This will be achieved by supporting perinatal leadership teams to create and craft the conditions for a positive culture of safety and continuous improvement, have a positive impact on the experiences of women, families and babies and enable a more collaborative, supportive workplace.
Expected outcomes:
- Improvement in safety and culture at Trust and system level as defined by local plans and system agreement.
- Improved staff satisfaction / experience for those working in maternity and neonatal services.
- Improved outcomes for women and babies as a result of good perinatal safety culture.
To keep up to date with the latest information please join our FuturesNHS page
Avoiding Brain Injury in Childbirth (ABC) is a national initiative commissioned by the Department of Health and Social Care, the Royal College of Obstetricians and THIS Institute. ABC aims to reduce avoidable brain injuries during childbirth by through improved clinical practice, teamwork and communication. The programme includes evidence-based tools, structured training, and protocols to support professionals in delivering safer, more personalised care. The ABC approach focuses on two high-risk areas:
- Detecting and responding to intrapartum fetal deterioration during labour (IFD)
- Managing impacted fetal head at caesarean birth (IFH)
Resources
Improving equity, diversity and inclusion in our maternity and neonatal workforce – Caroline Finch
Reflective blog from the Local Neonatal Unit Away Day – Caroline Finch


