Reflections on the Mental Health Safety Improvement Programme

In this blog from Stuart Kaill, Programme Development Lead for the Patient Safety Collaborative (PSC) at Health Innovation Manchester (HInM), he discusses the work of the Mental Health Safety Improvement Programme (MHSIP) as it nears the end of its commission later in 2023.
Mental Health Safety Improvement Programme (MHSIP) is a national patient safety programme commissioned by NHS England and NHS Improvement. It aims to improve patient safety and experience in mental health, learning disability and autism inpatient services, and specifically to reduce restrictive practices. Health Innovation Manchester has worked in collaboration with the Advancing Quality Alliance (Aqua) on this project across Greater Manchester.
Restrictive practice refers to any act which involves restricting a person such as physical restraint, the use of rapid tranquillisation, or the use of a seclusion room. Restrictive practices cause both physical and psychological harm to patients and can cause distress to an already vulnerable patient group. Lower levels of restrictive practice can significantly improve the experiences of both patients and staff.
The MHSIP involves rolling out a tried and tested change package for reducing restrictive practice (RRP), based on a pilot undertaken by the National Collaborating Centre for Mental Health, to bring about systematic and sustainable improvement in patient safety by utilising quality improvement approaches and methodology.
On 14th September 2023, ward teams from the MHSIP came together, online, for one last time to celebrate the end of the programme. This blog will give a summary of proceedings and the presentations given by the various speakers. Wendy Stobbs, Head of Programmes for the PSC at HInM opened the event and explained the national context in which the MHSIP has been developed and delivered, also taking the opportunity to promote membership of the Health Foundation’s Q Community. For many staff participating in the programme, this will have been their first foray into the world of quality improvement (QI). Joining the Q community can be a great next step on an individual’s QI journey, forming new networks and opening up new opportunities to develop professional areas of interest.
Paul Greenwood, Mental Health Programme Manager at Aqua, whose role in the programme has been coach and expert faculty, turned participant’s attention towards sustainability of QI work going forward. Opportunities to get more involved with QI and develop skills include:
- Establishing or joining QI collaboratives within organisations
- Linking in with organisational QI teams
- QI courses offered by Aqua to their members
- Joining the already mentioned Q Community
Paul also took the opportunity to raise awareness of the recent national data review for inpatient mental health services.
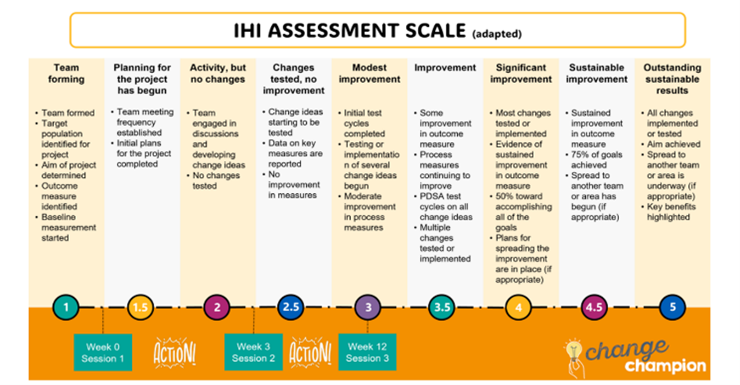
Picking up the theme of further QI opportunities, Tracy Mellor, Senior Improvement Lead at Pennine Care, took to the screen to give a brief overview of the work of the QI team based in her organisation. Tracy talked about some changes that the QI team are testing to improve their own ability to support teams undertaking QI work within their organisation. These changes include the adoption of the IHI’s project maturity scale to give everyone, from board to ward, a common understanding of how QI work progresses and help the team to target their support more effectively. It’s great news for ward teams at Pennine Care to know that they can feel supported on their QI journey and that the organisation ‘has their back’.
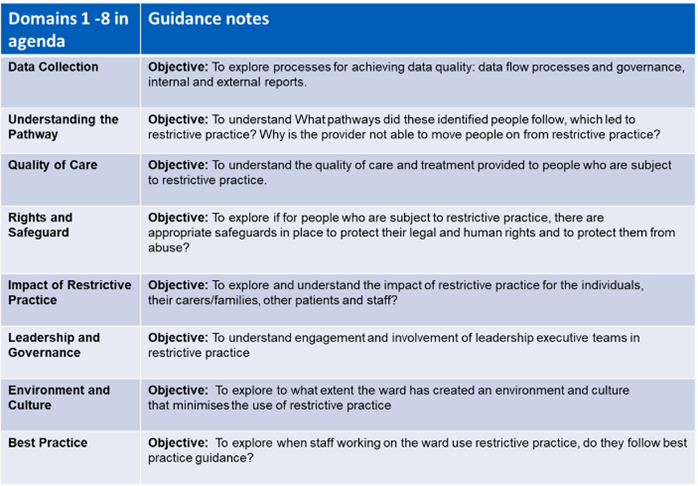
Joe Jones from Greater Manchester Mental Health NHS Trust (GMMH) picked to explain the work that their QI team has also been doing internally to work on RRP. Joe shared NHS England’s diagnostic tool which has been used to help ward teams identify gaps that might need addressing to enable successful QI.
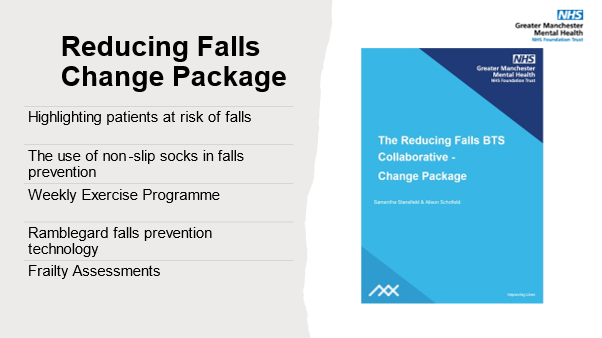
The GMMH RRP programme still has some way to go but already, they have developed a number of change ideas that will be tested in their collaborative. Ultimately, the GMMH RRP collaborative are working towards developing their own change package which will capture their own local ‘recipe for success’ to allow the work to be spread internally or even beyond.
Keeping with the theme of sustainability and future opportunities we turned our attention to the new Patient Safety Incident Response Framework (PSIRF). PSIRF will become enshrined in law next year and replaces the Serious Incident Framework (2015). The PSIRF has 4 main aims which are:
- Compassionate engagement and involvement of those affected by patient safety incidents.
- Application of a range of system-based approached to learning from patient safety incidents.
- Considered and proportionate responses to patient safety incidents.
- Supportive oversight focused on strengthening response system functioning and improvement.
So going forward, PSIRF will put QI front and centre of the approach to improving patient safety and we can expect QI work of the future to be influenced much more by themes that emerge from incident data. This video by NHS England explains more.
Jo-Anne Padget took over next to explain what PSIRF means, in practice for GMMH. Jo-Anne explained how the organisation has been engaging with a wide range of stakeholders to develop their own particular plan. Jo-Anne shared a couple of examples:
- She referenced self-harm as a ‘low-level’ incident that happens very frequently but wouldn’t normally warrant a full investigation but, under PSIRF, could be identified as an area where more learning and improvement could be generated by more in depth investigation.
- Jo-Anne also talked about their local Reducing Falls collaborative as an example of how improvement has been achieved by focussing on learning and improvement rather than repetitive Root Cause Analysis and action plans.
- Other examples of improvement priorities that have been informed by safety incident data include improving physical health, care of the deteriorating patient and suicide and self-harm.
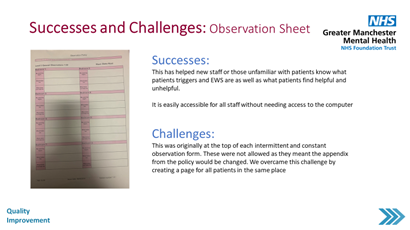
Next up we welcomed Erin Grinyer, a charge nurse and QI champion at GMMH. Erin presented a retrospective of the changes and results that they have worked on while participating in the programme. Among the plethora of ideas and learning that Erin shared, an example of a successful change was the introduction of an observation sheet that helps staff become more familiar, more quickly with individuals on the ward and avoid triggers that tend to lead to restrictive practices. Similarly, ward round sheets have been introduced to ensure continuity between shifts and therefore minimise patients’ frustrations. In addition to changes in patient care, the ward has been introducing ideas aimed at improving staff-wellbeing. These have already led to staff feeling more appreciated and valued and this in turn changes seen changes in the way staff engage with patients.
Crucially, Erin talked about the team’s realisation that all staff need to be involved in introducing and testing changes, so over the past year, they have made great efforts to get more staff involved in their QI work, increasing buy-in, increasing diversity of ideas and contributing to everyone’s professional development.
Marie Turner, Prof lead for RRP (Pennine Care) talked about their work at a 45 bedded low-secure service for males. This team joined the programme following a recognition that the service could do better around reducing restrictive practice. A key challenge that Marie referenced was around some of the longstanding assumptions and anxieties around the perceived need for restrictive practices and that reducing restrictive practices would make the wards ‘less safe’. Many of the changes tested centred around the addressing of unwritten rules. Another key improvement has been around how the service uses its own data to reflect back use of restrictive practices in real time and enable everyone to understand whether how they are doing with RP. Impressively, the service are also introducing a 10 day training plan, delivered over 5 weeks to improve awareness, attitudes and practice.
Following a quick comfort break, attendees participated in a collective stocktake exercise using a SOAR analysis. SOAR comes from the school of thought known as Appreciative Inquiry which provides an asset-based approach to change in organisations. As opposed to a deficit-based approach which would aim to ‘fix what’s wrong’ and asset-based approach looks to build on and do more of what we already have. SOAR is the Appreciative Inquiry take on ‘SWOT’ and SOAR stands for Strengths, Opportunities, Aspirations and Results.
This led us nicely into the final section in which Paul Greenwood presented each participating team with a special and unique award, with musical themes. A bit of fun but also an important recognition of how each team brought something very different to the table.
Wendy Stobbs returned to close the event. Although HInM’s commission for this work comes to an end at the end of September, teams are encouraged to stay in touch with HInM, Aqua and the national team and to look out for the new Mental Health, Learning Disability and Autism (MHLDA) inpatient programme from NHS England. Finally, hopefully we’ll see some of the teams getting well deserved nominations at next year’s round of health service awards! And that’s a wrap! A real uplifting and inspiring final learning session. HInM would like to wish lots of luck to everyone who has been involved, thank you!
For further information:
Join the Health Foundation’s Q Community and take your next steps on the Quality Improvement journey
Find out more about the Patient Safety Incident Response Framework (PSIRF) at Health Innovation Manchester
Find out more about the Mental Health Safety Improvement Programme at Health Innovation Manchester


