Insights and Reflections from the Maternity Safety Conference

The Maternity and Neonatal Safety Improvement Programme (MatNeoSIP) at Health Innovation Manchester, in collaboration with the Local Maternity and Neonatal System (LMNS) as the maternity and neonatal arm of NHS Greater Manchester (GM), hosted a Maternity Safety Conference on the 6th August 2024 in Manchester to share local maternity providers’ examples of innovation and good practice. Joining on the day to give a keynote address was Kate Brintworth (Chief Midwifery Officer for NHS England) and Donald Peebles, (National Clinical Director for Maternity at NHS England). As one of the National Patient Safety improvement Programmes, the MatNeoSIP aims to improve the safety and outcomes of maternal and neonatal care by reducing unwarranted variation and provide a high quality healthcare experience for all women, babies and families across maternity and neonatal care settings in England and reducing the number of maternal and neonatal deaths and harm.
The event was attended by midwives from across the GM system, bringing enthusiasm, energy and expertise to the day. The presentations given demonstrated real passion to drive improvements in care and outcomes, with a strong focus on addressing inequity and on tackling challenges with safety culture in the workplace.
“This event showcased all the fantastic Maternity and Neonatal Safety work taking place across GM. The extent of which was so inspiring, creative and innovative. Midwifery and Neonatal teams were able to show how the teams in their organisations could drive improvement, reduce risk and improve safety. Congratulations to all the teams that presented” Dr Paula Bennett Health Innovation Manchester Chief Nurse
Reflections from the event
Natalie Qureshi and Cathy Brewster, GM Maternity & Neonatal Voices Partnership and Najima Khalid MBE and founder and director of Women’s CHAI Project.
Greater Manchester and Eastern Cheshire Maternity Voices were asked to co-produce a resource on preterm birth symptoms to make the information more accessible and user-friendly. Traditional advice on preterm birth has been too technical and difficult for some, particularly non-English speakers, to understand. Given that the average reading age in the region is nine, a health literacy approach was necessary to address existing inequalities. They collaborated with the Women’s CHAI Project, engaging women from diverse backgrounds through focus groups. These inputs helped co-create a leaflet that explains preterm birth signs in a clear, easy-to-understand format. It is important that the service user voice is at the heart of any processes within maternity and neonatal service to ensure that any output meet the needs of our communities
Karen Clough, Safety Lead Midwife, GMEC SCN
Importance that as a system we need to continue to share information one way that this is achieved is by the newly formed Safety Special Interest Group with the aim to support the network, collaboration and disseminate information to improve safety and outcomes. Learning needs to take place when events go right as this will have an impact on positively improving the culture. We need to be proactive rather than reactive.
Bev O’Connor, Head of Midwifery at St Mary’s, Sarah Owen, Head of Midwifery at Wythenshawe and Esme Booth, Head of Midwifery at North Manchester
Gave an overview of process and quality improvement initiatives put in place following CQC report with the aim of improving culture and safety:
- Cross site capacity used to prevent prolonged delays
- Increased caesarean section capacity
- Enhanced collaborative working with MVP’s
- Improved access to translation services supported by the Cultural Safety Midwife.
- Improved staff moral – reduction in midwifery turnover, appointed 3 site-based retention midwives
- Staff attending Professional Behaviours and Patient Safety workshops to build confidence to challenge unprofessional behaviours.
- Extensive programme of engagement and listening events for all staff
- Civility Saves Lives workshop attended by all staff.
- Quarterly Happiness menti-meters used as a temperature check of staff feelings and morale.
- Supporting 26 international midwives
Importance of involving and listening to staff as together you can make a difference.
Caroline Finch, Programme Development Lead for the Maternity and Neonatal Safety Improvement Programme.
An overview was given on the aims of the 2023/24 programme and the economies of scale regional approach taken in collaborating with Health Innovation NW Coast and the Northwest Neonatal Operational Delivery Network (NWNODN) to support units with the implementation of perinatal optimisation QI initiatives. Subsequently this approach had achieved over 1000 hours of learning from Special Interest Groups that had been held, 500 plus hours of CPD from a regional study day with over 95 attendees, and development of resources that had been taken on board nationally. A highlight of some of the impact that had been seen within GMEC was:
- Antenatal steroids were 8% above the national average of 50%
- Intrapartum antibiotics had double over the 12 months to 30%
- Optimal cord management had seen an increase of 12% and above the national average of 66%
- Total number of interventions given had seen an increase from 55% to 64% and from a national context GMEC remains the highest performing region for this intervention,
The early recognition and management of deterioration in women and babies focus being on the implementation of the national Maternity Early Warning Score (MEWS) and the Neonatal Early Warning Trigger and Track (NEWTT2) within our paper-based maternity and neonatal providers had seen Oldham supporting the initial phases of the pilot and Macclesfield being the first provider to implement both MEWS and NEWTT2 nationally. Additionally, Tameside have also successfully implemented NEWTT2. Perinatal MDT approach is essential in embedding and sustaining changes in practice to improve outcomes for our preterm babies and birthing women.
Catherine Nash, Quality Improvement Lead Nurse, NWNODN
An overview of the three main data tools used within neonatal services which are:
- Exception reporting tool which will address all babies that are not born in the right place for gestation
- Improved optimisation tool developed to support providers with their MatNeoSIP data which will enable them to identify gaps in the data, increase awareness of the measures and highlight areas’ where QI initiatives would benefit the outcomes.
- Improved NWNODN dashboard which has an optimisation tab for showing regional, locality and unit quarterly outcomes and SBLv3 element 5 tab.
Accurate data inputting is essential
Chloe Hughes, Lead Midwife for SBL and Fetal Surveillance and Steph Birks, Neonatal Nurse and East Cheshire NHS Trust
East Cheshire implemented the national MEWS and NEWTT2 on return of onsite services and some of the challenges that they encountered was a change in what they believed to be historic normal level is now a trigger which has led to a perceived increase in workload and desensitising action. Inconsistencies around the use of the escalation and review sticker and lack of rationale for commencing neonates on the chart. The highlighted successes were that the tool was of a familiar format and when a score triggers an escalation, it makes the most experienced practitioner question findings and undertake a full risk assessment and they have implemented the tools across the trust. Process have been put in place to address the challenges experienced with training across the trust, key team members attending the ALERT course, auditing compliance, having champions within each area. All staff need to attend a behaviour workshop which focuses on escalation behaviours, impact of poor attitude, how the score can be improved and how to escalate or reassure the woman, family or healthcare professionals. Ensure all staff have completed training, important to have champions with each area and accept help and support when offered
Tony Kelly, Consultant Obstetrician and National Speciality Advisor NHSE, and Hannah Rutter, RM and QI Lead, Perinatal Deterioration, NHSE.
Tony highlighted that numerous reports have highlighted that recognition and management of deterioration continues to be an issue within maternity and neonatal services:
- Difficulties identifying, escalating and responding appropriately to deterioration
- Miscommunication and a lack of standardised processes with a plethora of different tools in use nationally
- Real need to improve recognition, management, and communication of risks
- Care provided to pregnant women and babies in a wide range of clinical settings
Deterioration will continue to be an issue as we are not learning and often try and fix the ‘wrong’ thing, with insufficient emphasis on the impact of culture and there has been no national standard tool/pathway. Development of MEWS considered the physiological parameters from conception to 4 weeks delivery, additional concerns were also included to address if staff, patients and family had any issues or other physiological aspects that are not included in the observations. The tool also has a clear thresholds and triggers to aid staff with escalation of concerns to appropriate MDT. NEWTT2 took on the same format and was developed in collaboration with BAPM. Implementation within paper-based sites has seen 19 go live with MEWS and 26 go live with NEWTT2 nationally.
The digital specification is taking a 3-phase approach and is currently coming to an end of phase 2 with phase 3 addressing identification of digital pathfinder sites to implement the digital specifications. Have a national standardised tool for both maternity and neonates will improve outcomes and reduce morbidity and mortality.
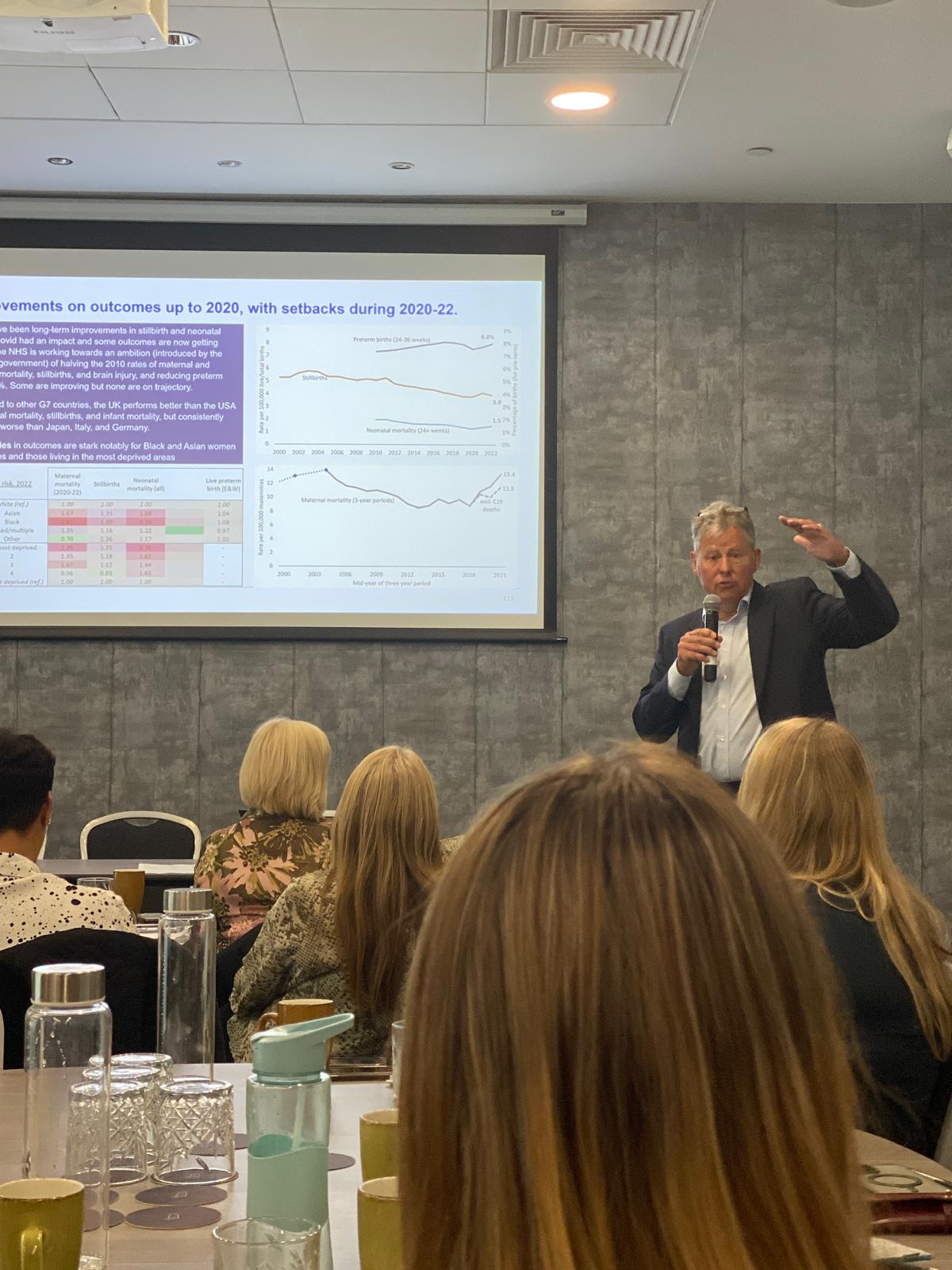
Kate Brintworth, Chief Midwifery Officer for England and Donald Peebles, National Clinical Director for Maternity NHSE
Kate and Donald discussed the current challenges facing maternity services with increasing complexities with pregnant women increasingly high risk, more premature babies which leads to more interventions and complexity with caesarean rates increasing up to 39.4% in 2022/23 from 48% in 2021/22. Antenatal and postnatal intervention are improving which leads to increased survival and rise in activity within our neonatal units.
The national ambition to half the rates of maternal and neonatal mortality, stillbirths, and brain injury, and reducing preterm birth to 6% has been impacted by the COVID pandemic with none on target of reaching these ambitions. A plethora of reports continue to highlight the stark inequalities in outcomes for Black and Asian women and those living in the most deprived areas. With the new government its manifesto clearly addressed the importance of focusing and acting on these disparities.
Progress has been made on the four priorities in the three-year plan which defines how we can make maternity and neonatal care safer, more personalised and more equitable:
Listening: Latest service user survey shows improvement in 7/10 areas and published guidance for involving service users to improve care.
Workforce: Record number of midwives in post, increased number of neonatal nurses and significant increases in other workforce groups. Every unit now has a retention midwife which is contributing to a reduction in leaver rates.
Culture: All maternity and neonatal providers senior leadership team have started the perinatal culture and leadership programme and additional support for trust that require through the Maternity Safety Support Programme (MSSP).
Standards: Good practice standards for care, training and new neonatal service spec and investment in additional neonatal cots.
Service users are our biggest allies in making change happen.
Chloe Hughes, Lead Midwife for Saving Babies Lives & Fetal surveillance/GMEC Project Lead for Each Baby Counts Learn and Support/Project Midwife for the ABC Collaboration and Professional Midwifery Advocate, East Cheshire
Chloe was seconded to implement EBC escalation tool kit and interventions into maternity providers within GMEC as there was a need to have a standardised approach to clinical escalation for maternity staff. A behaviour workshop was delivered to 2000 doctors and midwives across GMEC which looked at how do we escalate, the language used, how we document, barriers to effective escalation, escalation behaviours and solutions. Some of the examples to the solutions were:
- Safety huddles
- Use of clear and concise language
- Make it clear you are escalating civility
The EBC toolkit include three interventions: Teach or Treat; Advise, Inform, Do (AID) and Team of the Shift, with the AI of reducing delays in escalation by improving the response and action taken, standardise the use of safety critical language, reduce feelings of hierarchy and create a supportive environment, promote culture of respect and civility amongst staff and improve the way we listen to women. We cannot keep failing at escalation.
Deborah Buxton, Lead Midwife for Intrapartum Services and Northern Care Alliance.
In 2023 the Maternity Improvement Program (MIP) was commenced with the aim of developing the labour ward coordinators with bespoke 12-month programme. The focus was on shaping and maintaining an inclusive, compassionate culture, co-creating a collective service ambition and team objectives, ensure colleagues are engaged, skilled, educated and motivated and to promote the trust values. The programme includes attendance on the NCA Accelerated Leadership Course, quarterly progress and wellbeing check-in’s, exposure to the strategic network with 1:1 with Director of Midwifery, coaching and quality improvement sessions. Coordinators realising what their jobs are and given the opportunity to develop
The Fern Team, Wrightington, Wigan and Leigh Teaching Hospitals NHS FT
The Fern team are a team of community midwives and support workers providing enhanced care to women living in the most deprived areas of the borough, non-English speaking women and asylum seekers. One of the initiatives that they have implemented is a Non-English Speaking (NES) pass that is issued to all women who do not speak English and require an interpreter for appointments with the overarching aim to reduce inequalities for the most at-risk women and to break down barriers to accessing emergency care. We need to find ways of reducing inequalities by making our service more accessible.
Stockport NHS Trust
Idea came in response from service users’ experiences of the induction of labour process which led to collaboration with the Maternity and Neonatal Voice Partnership. A survey was conducted to establish priorities for actions that would positively impact women and families to ensure that all were receiving the same evidenced based information in the antenatal period prior to induction. A 17-page booklet (the passport) was produced and launched in January 2023 which has seen a reduction in induction of labour rates from over 40% to 30%. Women need to be involved in shared decision making to enable them to make an informed choice.
Leanne Ingle, Practice Retention Midwife, Tameside and Glossop Integrated Care
The Curiosity Café was established in the summer of 2023 with the overarching aim of staff co-creating a better working environment and future together, making Tameside the best place to work, learn and develop. This has led to development of 4 types of Curiosity Cafes: Static café; Mobile café, Online café and Themed cafes. The Involving staff will have positive impact on the service.
Alexa Hunt, Lead Midwife for Maternity Tobacco Dependency Service (MTDS)
Research has shown that the risk of stillbirth is 52% higher in pregnant women who smoke therefore it vital that women are supported to have a smoke free pregnancy. In 2022 Alexa came into post as the Lead midwife for MTDS and recruited new members into the depleted team. Through implementing changes within the service, they have been seeing a reduction of smoking at time of booking from 683 women in 2021 to 507 women in 2023, and a reduction in ‘smoking at time of delivery from 10.8% to 6.5%. Women need to have an effective service that will support them to quit smoking.